As healthcare consumers, we are at a distinct disadvantage understanding what we are buying and how much it costs. Perhaps those who are fortunate enough to have good, comprehensive health insurance haven’t been caught off guard by the cost of a medical service. However, anyone who is uninsured or underinsured has probably experienced sticker shock at least once.
Furthermore, most of us have no information about either the price of a healthcare visit or procedure or how it compares to that of another hospital. As an example, National Public Radio reported on the experience of one man in Florida who got two abdominal CT scans at different locations near Fort Myers. His first scan cost almost $300. The second was almost 30 times more expensive—nearly $9,000. After his insurance covered its share, he still faced a bill for $3,394. [1]
New CMS Rules for Transparent Healthcare Pricing in 2021
Our payment and reimbursement system has very little, if any, price transparency for patients, which is why the Centers for Medicare and Medicaid Services (CMS) released rules to provide greater transparency into hospital procedure and services pricing. Starting in January of 2021, hospitals were required to make public their standard charges in two ways: (1) as a comprehensive machine-readable file; and (2) in a consumer-friendly format.
For the consumer-friendly format, hospitals have two options:
- Publicize payer-specific negotiated charges, discounted cash prices, the de-identified minimum negotiated charge, and the de-identified maximum negotiated charge for 300 “shoppable” services such as a knee replacement or a chest x-ray.
- OR offer an internet-based price estimator tool for selected shoppable services in a consumer-friendly format. There are some specific caveats: it needs to be easily accessible on the hospital’s website and cannot require a user to register or establish a user account or password.
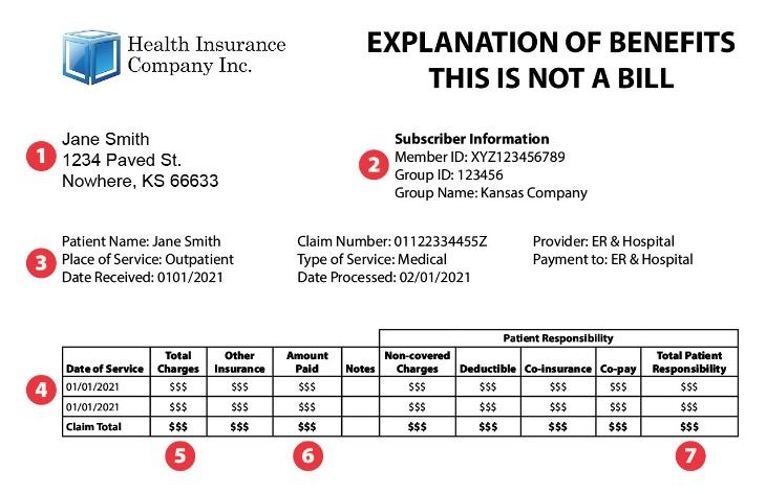
The idea is to let consumers make informed decisions about where to get care by giving them healthcare pricing information in advance, while they still have choices. This contrasts with the traditional health insurance Explanation of Benefits (EOB), which contains information about charged amounts, covered amounts, co-pay and co-insurance information, and an estimate of what you might owe the provider or hospital. You get these after the services have been delivered – too late to decide how your healthcare dollars should have been spent.
Are Hospitals Complying with the New Price Transparency Rule?
So, how well are the new CMS rules working? I did my own test and went to three hospital websites to assess the following:
- Could I find the machine-readable files?
- Could I access and use the files?
- Were the cost estimators easy to use?
Here’s my summary:
- Once I figured out what to search for on a website, the files were easy to find. I used the terms “CMS price” or “price transparency.” The data is often found under the billing section of the web
- Some files were easier to access than others. In one instance, I would’ve had to be a database programmer to access the data in the file.
- Only one site I went to made it easy to figure out a cost estimate. Others required me to enter information about my insurance and were gated by a “click if you’re not a robot,” which is prohibited under the CMS In one case, I could get to the data, but only after I logged into my patient portal account.
- For a standard cardiovascular stress test, I found the following prices: $1,680, $3,071 and $810. That is a 380% price differential across 3 hospitals all located in Massachusetts.
Based on my small survey, it’s not surprising that less than 6% of hospitals are fully compliant with the federal requirement that health systems publicly disclose the prices they charge for medical care. This was confirmed by a study done by Health Affairs.
This has led the federal government to propose a new CMS rule, which increases fines to non-compliant hospitals. These could amount to up to $2M a year for each large hospital that is found to be non-compliant – versus the current $109,500 annual cap.
Similarly, CMS finalized its “Transparency in Coverage” rule, which will go into effect in January of 2022. It requires that payers provide similar information to their provider counterparts. Requiring both payers and providers to share similar information should allow patients to cross check the information with their health plan, leading to even greater transparency.
Many hospitals didn’t comply because the cost of implementing the required changes were potentially higher than the cost of a penalty. Furthermore, some hospitals are reluctant to share their prices. CMS hopes that an increase in the maximum penalty by twentyfold will be enough of a stick to get hospitals moving.
Better Information, Better Healthcare Consumers
CMS’ intentions are good. They hope that by providing us with better information about the price and cost of healthcare services, we might become better consumers. I am hopeful that organizations interested in price transparency, such as advocacy groups or policy researchers, will accumulate the data from all the hospitals in each market and provide some understanding of trends they are seeing. This should also allow employers to use the information to better negotiate with their health plan to create cost effective product design or use incentives to drive enrollees to lower cost setting.
From my perspective, liberating that data is a great idea – but it must be user friendly, easily accessible, and actually have an impact.
[1] https://www.npr.org/sections/health-shots/2018/04/09/598794123/bill-of-the-month-a-tale-of-2-ct-scanners-one-richer-one-poorer