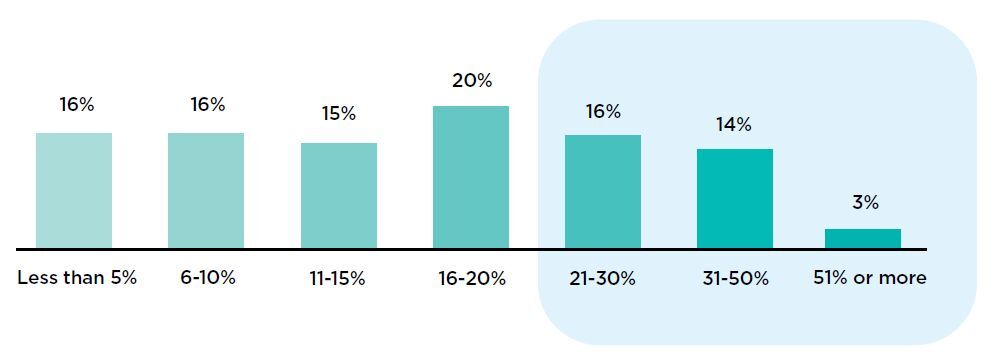
Even though improving the quality and robustness of provider data has become a top priority for healthcare organizations, many still believe their data quality is low. As shown in the figure below, one third of the respondents to a HIMSS survey1 of healthcare executives said that 21% or more of their organization’s provider directory data is of poor quality.

Why should you invest in improving your provider data?
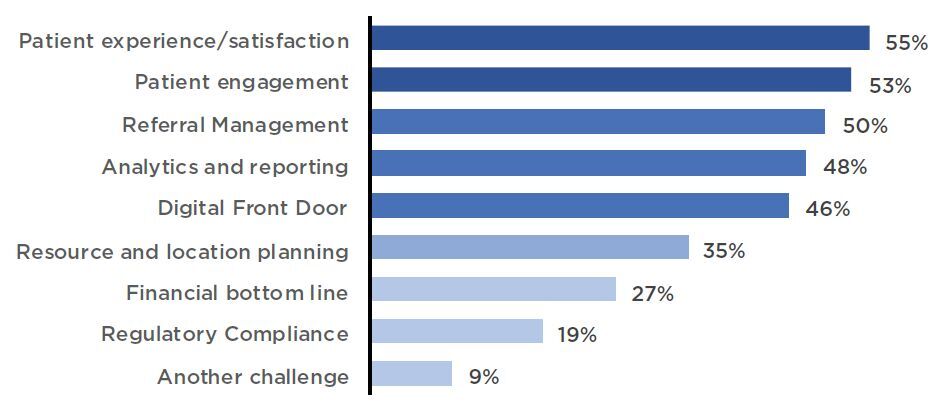
When we look at top priorities for health systems, many of them rely on having good, clean provider data. When asked, which of the following are challenges or barriers that you are trying to solve for with your provider data management system? The top answers were:
- Improving patient experience/satisfaction
- Patient Engagement
- Referral management – which is about revenue growth.
Improving Patient Experience & Patient Engagement
Today’s consumers are not shy about voting with their feet, so if they have a bad digital experience interacting with your provider directory, they may just move on to the next provider that makes it easier. As patients interact with different entry points into your organization, physical and virtual, they expect the same experience with each. But that isn’t always the case. Often, because of data limitations, the digital front door is not as welcoming as the lobby. Cleaning up your provider information can be the first step in improving that experience, since the first step through the digital front door is often looking for provider information.
Provider Data Management is key to meeting business goals, HIMSS, Decemeber 2022
Referral Management – Generating Revenue
Good provider information can help guide referrals, keep patients in network and preventing leakage. If your referral coordinator has bad information about which specialists are in network, and your patient gets sent to them, the financial implications are significant. The patient might get charged out of network costs, which could lead them to leave your practice. You’ve also missed the opportunity to keep them in your health system’s network and earn revenue for that visit.
Referral leakage affects a hospital’s financial health. The cost of referral leakage for health care systems in the United States is estimated at upwards of $97 million for every 100 affiliated physicians, which contributes to a 20% loss of a health care system’s annual revenue. In fact, a recent healthcare innovation article noted that most health care systems lose an average of $200 to $500 million to competitors each year due to outward migration of patients.
Regulatory Requirements – Keeping the Unexpected Costs at Bay
Although not high on the list of responses to the HIMSS survey, an unexpected audit and a fine can really set your organization back. For payers and providers the provider directory provisions of the No Surprises Act, calls for accurate provider information and potential costs for both payers and providers. For health plans, inaccurate data can lead to problems with Network Adequacy or fines from the State and Federal government. Regulations enable CMS to fine insurers up to $25,000 per Medicare beneficiary for errors in Medicare Advantage plan directories and up to $100 per beneficiary for mistakes in plans sold on HealthCare.gov
If you think about the many activities that require provider information – scheduling, referrals, billing, analytics and reporting, consumer engagement and many more – it’s surprising that more organizations haven’t invested in clean provider data.
Why is managing provider information so difficult?
Leaders in healthcare organizations often don’t think about the true complexity of provider information. Yet, if you think about it in the context of a connected ecosystem, there are many relationships.
Provider Directory Relationships
• Relationships are complex. There is the relationship between providers and their organizations, and providers and health plans, and then the layers of how those all relate to one another. For example, a provider that is part of a large health system might also belong to an Independent Physician Association (IPA), which contracts on their behalf with multiple payers. However, not every provider in the practice may be an IPA member and therefore has different relationships with different payers.
.

• The source of the data matters. An address associated with a claim might be the billing address, where to send information about payments, which can be very different from the location where a provider practices. That practice address can be different depending on the day of the week! Credentialing information might exist in multiple places, but the credentialing system should be the only source of truth.
• The data represents people. People don’t always have simple relationship structures. For example, an OG/GYN may practice 4 days a week in a private practice office as part of a large Integrated Delivery Network (IDN). She accepts Commercial, Medicare and FFE, but not Medicaid. On Fridays she practices at a Federally Qualified Health Center, accepts all the previous insurance plus Medicaid and has a translator to support the multiple languages spoken by the patients. Capturing even part of that complexity requires a data model that understands how a provider really practices.
• The data come from multiple sources. Not all of the information you need to create a complete view of a provider exists in one system. Often there are many source systems that contain that information. Perhaps the Human Resources system has information about licensing and where the provider got their degree, but there’s an entirely different system that has data about where to send billing information.
I need to improve my provider data management strategy, now what?
As previously mentioned, providers spend a lot of resources – people and dollars – to keeping their provider information up to date. With better systems, technology, and processes, that could mean a direct improvement to the bottom line. Often, organizations take a low-tech approach to solve the problem, only to realize that they aren’t getting the improvements they anticipated.
Here are some key steps in your journey to improve your provider data:
- Map your business strategy to your provider data management strategy –are there gaps
- Create a set of scenarios that require good clean provider information.
- Develop a cross-functional provider data governance working group to assess the challenges and work toward solutions.
- Identify all the sources of provider data within your organization. What systems do they come from? What data do they include?
- Work with InterSystems. We can create the single source of truth for your provider data and meet your key consumer scenarios.
We have a proven solution that has been deployed by some of the largest health systems and payers in the world. InterSystems can advance your organization to actively solving the problem – not just thinking about it.
1 - Provider Data Management is key to meeting business goals, HIMSS, Decemeber 2022


























