They’ve been upgrading the elevators in our building for most of this year. In theory, this means the whole system is getting more efficient. In practice, it has meant slow service and confusion as new and old systems coexist poorly together. Sort of like the current hybrid business model we have today in the U.S. healthcare system as we “upgrade” from fee-for-service (FFS) to pay-for-value.
Think about it. FFS has a known set of rules. Everyone understands how the rules work, and the system is predictable. However, we also know that the FFS payment model is not optimal. We don’t reward better outcomes, we often don’t coordinate care, and we incent excessive waste in the system.
Similarly, old elevators were a known quantity with predictable behaviors, yet also not optimal, especially around 9AM, noon and 5 PM.
And so, we’ve set out to fix them both, gradually replacing traditional elevators with so-called “ smart” ones. Replacing pay for volume, with its perverse incentives, with pay-for-value, and a whole new set of demands on providers to follow standard pathways, measure outcomes, coordinate services, move care to lower intensity settings, and keep people healthy. The challenge is that in most healthcare organizations, there is little rhyme or reason to patient and payment mix. Providers may see a fee-for-service patient at 9:15 and a pay-for value patient at 9:30 with the same condition, but totally different business rules governing care.
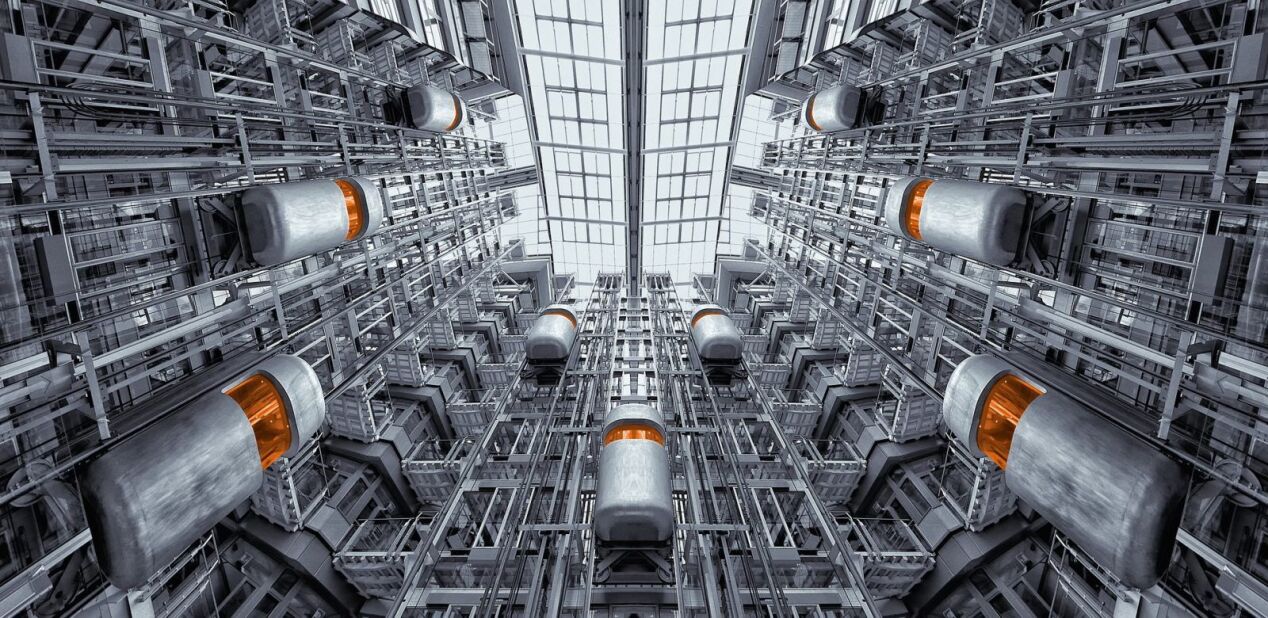
Our new elevators demand that you select your floor before entering, require that you swipe your badge before delivering you to your destination, and accept no change of plan en route – there are no floor selection buttons once inside. But since only one elevator is smart, another is out of service having its innards replaced, and the others follow the old system of enter-and-push-a-button, movement between floors has become an exercise in waiting, frustration, and confusion. Even the elevator company guys who rode with me recently were confused.
In the scheme of things, the elevators aren’t a big deal. Our healthcare system is, and the current transition to value-based is stuck between the old and the new. As a recent New England Journal of Medicine Catalyst article remarked, “providers can feel trapped, fearful of having a foot in two canoes.” There are not enough providers who deliver care under these the new models of care to feel hope.
Listening to chatter while waiting for an elevator two days ago, there were nothing but complaints about how this hybrid system was not working. However, I am sure that once we have converted to the new system, and have passed the tipping point, my colleagues will start to forget the pain they have endured during the transition. I’m optimistic that the same will be true for our healthcare system’s journey to more patient-centric, value-based care.